The FDA has approved an off-the-shelf cell therapy from Gamida Cell that makes life-saving treatment more widely available to patients with certain blood cancers. The new therapy could also help overcome some of the racial disparities that persist in accessing such treatments.
The regulatory decision announced Monday covers the treatment of patients 12 and older with blood cancers intended to be treated by an umbilical cord transplant. The Gamida Cell therapy, which was known in development as omidubicel, will be marketed under the brand name “Omisirge.”

At ViVE 2024, Panelists Share Prior Authorization Progress and Frustration in Payer Insights Program
At the Payer Insights sessions on Day 1 of ViVE 2024, a panel on prior authorization offered compelling insights from speakers who shared the positive developments in this area after years of mounting frustration. Speakers also shared challenges as they work with providers to figure out how policy developments and technology will work in practice.
Standard treatment for some blood cancers is the transplant of donor stem cells that reconstitute a patient’s bone marrow. The best source of these cells is a matched donor, typically a sibling. But matched siblings aren’t always an option, leaving some patients to rely on unrelated donors who are matched, half a match, or no match at all. The matching problem is particularly pronounced in underrepresented communities. For example, just 29% of Black patients can find an unrelated match in donor registries, Gamida Cell said in an April investor presentation.
Obtaining the cells from umbilical cord blood has expanded access to treatment without the need to find a match. However, this source provides low numbers of cells, which reduces the chances of transplanted cells being successfully taken up by the recipient’s bone marrow to make new white blood cells, what’s called engraftment.
Gamida Cell makes Omisirge from cord blood. But the company’s manufacturing process leverages nicotinamide, a small molecule that leads to enriched hematopoietic progenitor cells, descendants of stem cells that can differentiate into specialized types of cells. According to Gamida Cell research, ex vivo multiplying of the source cells in the presence of nicotinamide reduces cellular stress and preserves the ability of the cells to differentiate and engraft.
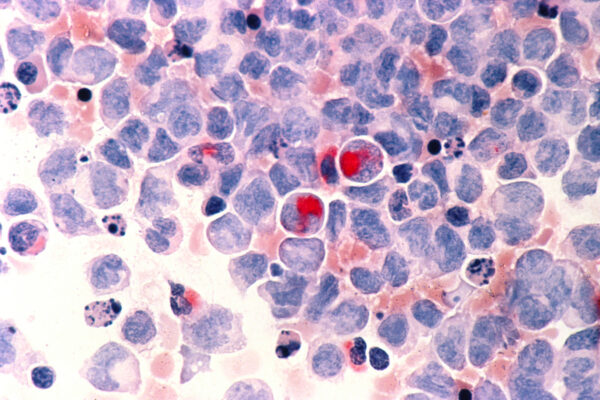
The FDA based its approval of Omisirge on the results of a Phase 3 study that enrolled 125 patients who had previously been treated for various blood cancers such as acute lymphocytic leukemia, acute myeloid leukemia, myelodysplastic syndrome, chronic myeloid leukemia, and lymphoma. The open-label study compared Omisirge to treatment with transplants of unmanipulated cord blood.

Using Informed Awareness to Transform Care Coordination and Improve the Clinical and Patient Experience
This eBook, in collaboration with Care Logistics, details how hospitals and health systems can facilitate more effective decision-making by operationalizing elevated awareness.
The study’s main goal was to measure the time to the engraftment of neutrophils, a type of white blood cell. According to the trial results, the median time to this neutrophil recovery was 12 days in the Omisirge group compared with 22 days in the control group. The cell therapy from Gamida cell was also better on the secondary goal measuring for infections. In the Omisirge group, the incidence of bacterial infections classified as grade 2 or 3, or fungal infections classified as grade 3, was 39%. In the control arm, the incidence of such infections was 60%.
Omisirge’s approval comes with a boxed warning that cautions of complication risks that include fatal or life-threatening infusion reactions, graft versus host disease, engraftment syndrome, and graft failure. The FDA notes that these warnings are similar to those of other approved umbilical cord blood products. The full Phase 3 results were published in 2021 in the journal Blood. Noting the cell therapy’s potential to address racial disparities, Gamida Cell said in its approval announcement that more than 40% of the patients in the pivotal study were racially and ethnically diverse. Stakeholders in the stem cell transplant sector have taken note.
“Patients who are Black or African American have just a 29% chance of finding a match via the donor registry versus a 79% chance for patients who are White,” Steven Devine, chief medical officer of the National Marrow Donor Program/ Be The Match, said in a prepared statement. “Adding Omisirge as a new donor source may help increase access to stem cell transplant for patients from racially or ethnically diverse backgrounds who struggle to find a fully matched donor in the registry.”
[Paragraph updated to correct status of GDA-201.] FDA approval of Omisirge came later than Gamida Cell initially expected. A January 30 target date for a regulatory decision was pushed to May 1 when the FDA asked for data from the Phase 3 study. That delay led to a corporate restructuring three weeks ago that included discontinuation of the company’s preclinical pipeline of cell therapies based on engineered natural killer cells. GDA-201, a natural killer cell therapy in development for non-Hodgkin lymphoma, is continuing Phase 1 testing.
Gamida Cell will discuss the Omisirge approval during a conference call scheduled for Tuesday, 8 a.m. Eastern time.
Public domain image of acute myelocytic leukemia from the National Cancer Institute












