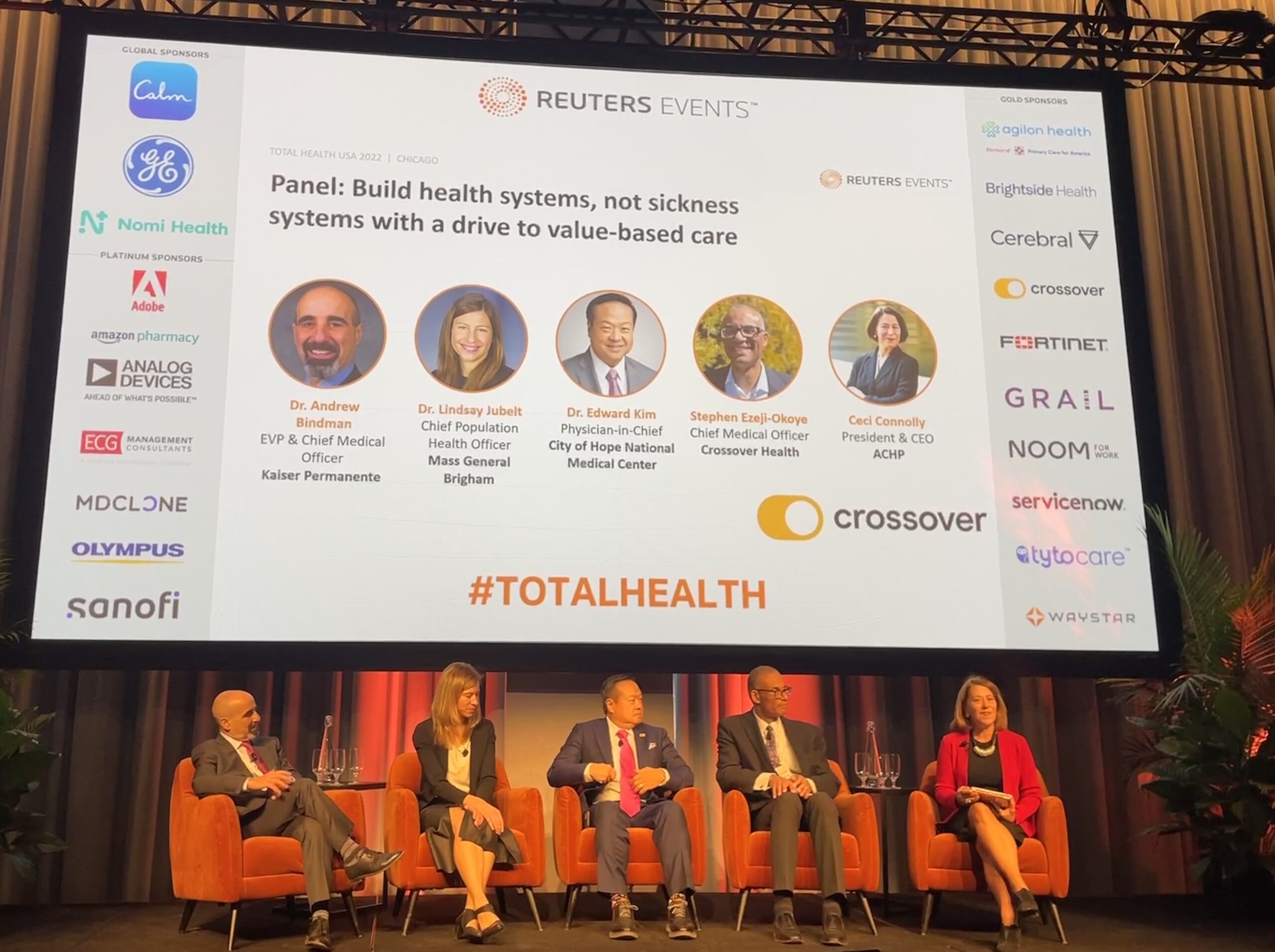
Health maintenance is in some ways overmedicalized in the U.S., executives from major health systems said Thursday at Reuters’ Total Health conference in Chicago.
The panelists agreed that treatments and procedures aren’t the only ways to support patients’ health and said that providers would be wise to place more emphasis on integrating social services into their care models.

At ViVE 2024, Panelists Share Prior Authorization Progress and Frustration in Payer Insights Program
At the Payer Insights sessions on Day 1 of ViVE 2024, a panel on prior authorization offered compelling insights from speakers who shared the positive developments in this area after years of mounting frustration. Speakers also shared challenges as they work with providers to figure out how policy developments and technology will work in practice.
“We fail at delivering some of the most basic care compared to other countries in the world — we are on the bottom of almost every indicator of health,” said Dr. Lindsay Jubelt, chief population health officer at Mass General Brigham. “And a lot of that is because we’ve over-invested in our healthcare systems and under-invested in our communities.”
As the healthcare industry begins to focus more on addressing social determinants of health, Dr. Jubelt urged health systems to spend more time advocating for funds to be sent to community partners and social programs, such as those focusing on healthy food distribution or improving air quality.
She pointed out that investments in social services have been proven to positively impact health outcomes.
“Countries that spend more on social services than healthcare have better health outcomes,” Dr. Jubelt said. “And then it’s true within the United States — states that spend more on social services than healthcare have better outcomes. We need to think about how we can solve that problem by being healthcare institutions and being advocates — the dollars going to the right place can really help our communities.”

The Impact Brands: Empowering Wellness Through Natural and Holistic Solutions
In an era of escalating healthcare costs and a growing preference for natural, holistic approaches to health, The Impact Brands emerges as a collective of diverse brands dedicated to supporting overall wellness through natural means.
Dr. Andrew Bindman, Kaiser Permanente’s chief medical officer, concurred. He encouraged health systems to not only make investments in social programs, but also integrate them into care delivery.
For example, Kaiser Permanente created a tool called Thrive Local, a platform that lets patients know what community resources are available to them. Physicians can also pull up the tool during appointments, just as they would with a prescription, and connect patients to resources in their neighborhood.
“It’s key not only to have these investments, but to make them integrated with how we’re delivering care so that we’re then in a position to be able to also see the value that has returned in terms of health outcomes,” Dr. Bindman said. “These could be differences like reducing cardiac events, cancer events and so forth — events we know are highly related to social causes.”
The U.S. healthcare needs to create payment models that allow providers to test different kinds of interventions and then measure health outcomes, Dr. Bindman declared. Once there is data within the EHR that validates the impact that social interventions have, he said there will be “very good reasons to believe” that community investments return critical value.
“We need a payment model that gives us the flexibility to ask ‘Is it better for us to think about providing an additional CT scan, or would it be better to invest in providing stable food for this patient with diabetes so that they can control their sugar more effectively and reduce the risk of getting a disease or needing an amputation down the line?’” Dr. Bindman said.
Community investments that focus on addressing social determinants of health is something Kaiser Permante is leaning “heavily” into, according to Dr. Bindman. Another example of a related program at the health system is its recent $50 million pledge to battle food and nutrition insecurity.
Photo: MedCity News












