
Using Informed Awareness to Transform Care Coordination and Improve the Clinical and Patient Experience
This eBook, in collaboration with Care Logistics, details how hospitals and health systems can facilitate more effective decision-making by operationalizing elevated awareness.
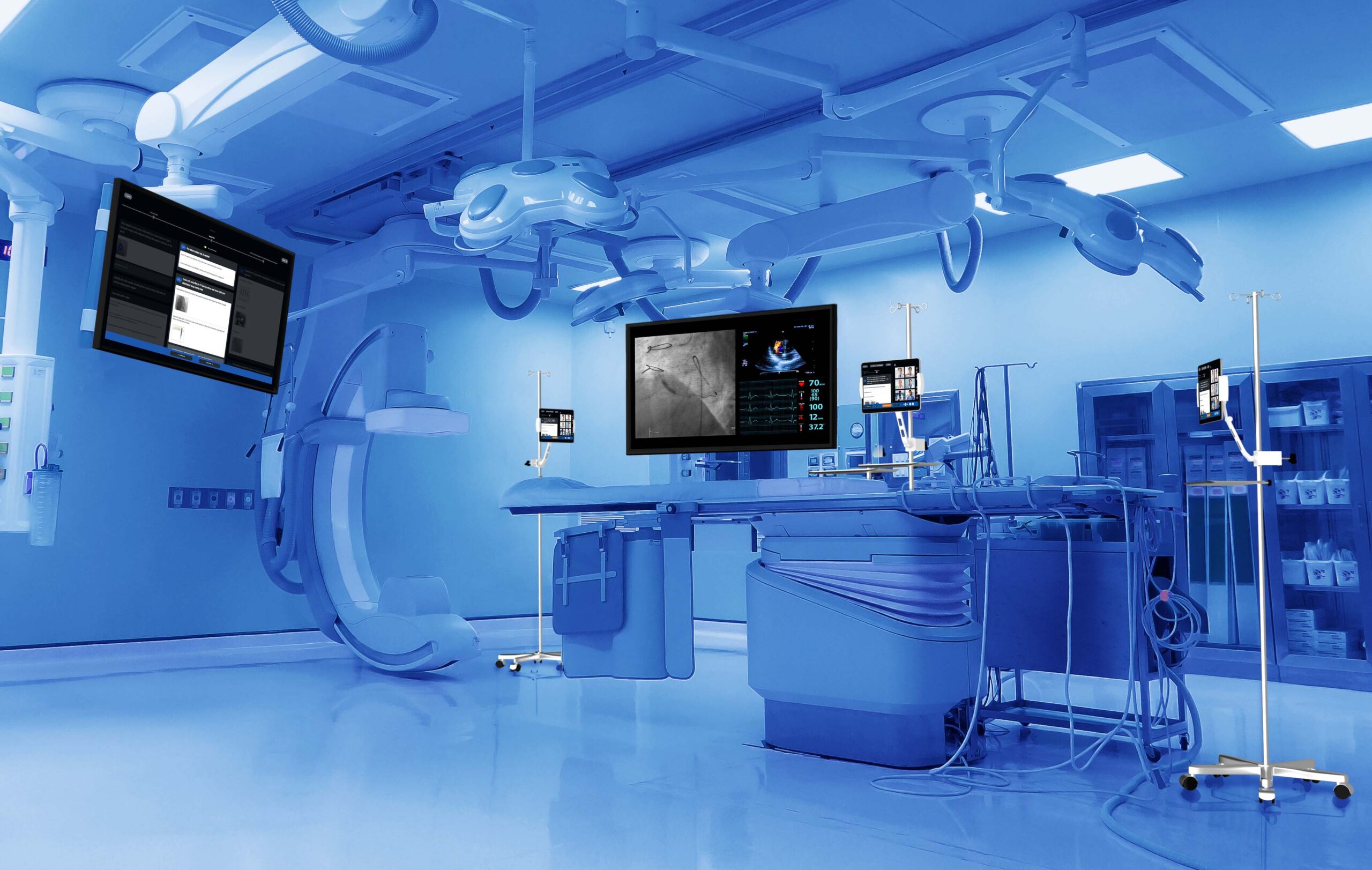
Observing surgical cases in person has long been a standard practice for purchasing and adopting new medical technologies and techniques. However, access to operating rooms, the cost and complexity of travel, patient privacy and safety, and other factors limit the utility of this approach. These limitations became particularly acute with the onset of the Covid-19 pandemic, which severely restricted access to medical settings.
An innovative approach known as remote case observation (RCO) addresses many of the challenges mentioned above, enabling physicians to access procedures remotely without the burden of travel. While challenges related to in-person observation have increased the adoption rate and the necessity for RCO, the benefits of this technology mean its use is likely to continue growing even after Covid-19-related disruption subsides. More than just a new technology option, it represents a paradigm shift in observing procedures. It provides a better experience for operating and observing physicians, poses less risk for hospitals and patients, and creates a broader adoption of life-saving innovations.

The Impact Brands: Empowering Wellness Through Natural and Holistic Solutions
In an era of escalating healthcare costs and a growing preference for natural, holistic approaches to health, The Impact Brands emerges as a collective of diverse brands dedicated to supporting overall wellness through natural means.
What is RCO?
Unlike traditional videoconferencing, RCO is purpose-built for any healthcare setting. A robust RCO platform has the following capabilities:
- Real-time procedure visualization: Provide live feeds of all imaging and diagnostic equipment. In most cases, a visiting physician would not have this up-close accessibility to all the equipment in the room.
- Procedural playbook: Provide a visual, step-by-step guide to the procedure, enabling everyone to stay on the same page, drive engagement, and communicate the latest best practices.
- Real-time collaboration: Ask and answer questions in real-time by communicating with a physician or including comments that would become part of the post-operative report.
- Low-latency Wi-Fi/LTE capabilities: Ensure interruption-free connectivity with options for areas with poor network coverage.
- Viewer controls: Enable remote viewers to choose from multiple viewpoints, zoom in and out as needed, and annotate on live imaging.
- Data capture: Gain structured insights into procedures and collect highly detailed data for clinical trials, device quality assurance, procedural analytics, and research data capture.
With a comprehensive, robust digital platform for RCO, clinicians, healthcare organizations, and medical device companies can not only break through the logistical limitations of in-person case observation — they can drive levels of engagement and learning that were previously not possible.
Helping Physicians Make the Most of Their Time and Expertise
For observing physicians, RCO serves as a “virtual cockpit” for any procedure. It allows physicians to see procedures in greater detail—and greater comfort—than on a monitor in a procedure. From a physician’s perspective and new hospital mandates limiting access to their facilities, having fewer people in the room has become the new normal. Allowing those who only absolutely need to be in the room reduces potential distractions, physical workflow disruptions, and exposure to contagions.
Using digital platforms for RCO, physicians can force multiply their access to educational opportunities and interactions with peers or collaborate on new techniques and technologies. It also provides physicians from all over the world the ability to learn new techniques or observe the use of technology without impacting their responsibility to their patients. With visualization of the entire workflow, known best practices, and procedural processes, introducing new therapies to their healthcare system may provide an easier transition and minimize the learning curve when bringing new therapies to their patient population.
Performance-tracking tools can provide physicians with real-time data that previously may have been limited and expensive based on having to be in the room as a procedure happens. Furthermore, it enables more observation in less time, which can reduce variability in device utilization, surgery workflows, and outcomes.
Increasing the Availability of Medical Innovation
RCO enables medical-device companies to standardize training, disseminate best practices, keep users current on the latest improvements and upgrades to technology, and the ability to capture data in new ways. Medical device sales representatives can ask questions during observation and interact with the proctor to familiarize themselves more with the product and gain deeper insights while also learning valuable techniques.
With a digital procedural playbook, sales teams can learn and share best practices, enabling them to expand their expertise and knowledge and allowing other team members to step in with minimal disruption at any point during a procedure. Medical device companies can also provide training assessments to evaluate and improve product and related procedural knowledge at the end of the procedure.
Reducing Risk, Cost, and Disruption for Hospitals
Hospitals need to keep patient safety and operational efficiency at the forefront. By minimizing the number of individuals entering the OR, RCO provides immediate operational and safety improvements. More broadly, it has the potential to reduce care viability, which may lead to improved outcomes, and enhance patient satisfaction, all of which can help drive down costs.
For every hospital, RCO lowers barriers to the adoption of new technologies. RCO can significantly accelerate the adoption of new procedures and any procedures that require regular proctoring and observation. Physicians can learn new techniques remotely that may improve patient care. For the trailblazing hospitals that adopt and disseminate new technologies, RCO enables them to bring innovative programs to a wider audience, increase their referral base, and potentially recruit physicians as a top-tier center of excellence.
With any new technology, hospitals must carefully consider the implications of cost and patient outcomes. Digital technologies introduced recently are compliant with privacy regulations and proven to be valuable to a physician; however, a layer of cost and complexity still exists with their use. A newer platform, such as Explorer Live, uses mobile devices, has a minimal footprint, and can be set up in ten minutes or less. Multiple network options can enable hospitals to manage bandwidth and deploy RCO in shielded locations. Remote users can install the observation platform on their desktop or mobile device. Platforms that align with current hospital privacy and compliance regulations enable easy accessibility for remote observers.
Reducing Barriers to Medical Innovation
Medical device companies can provide access to new innovative therapies and life-saving technologies in areas that previously were slow to adoption due to the geographical location of their providers. While Covid-19 continues to increase the sense of urgency for digital platforms like RCO, the advantages mean adoption is likely to continue growing after the pandemic is in the rearview mirror. It has the potential to reduce cost and risk, increase the availability of new procedures, and improve patient care through real-time access to education and support. Moving forward into the future, RCO may see increasing use in various contexts such as clinical trials, academia, medical education, and product development. Ultimately, patients will be beneficiaries of this pragmatic yet powerful tool.
Photo: Explorer Surgical
Jennifer Fried is the CEO and Co-Founder of Explorer Surgical. Jennifer founded the company with Dr. Alex Langerman as an MBA student at the University of Chicago Booth School of Business, where she received a degree with honors in Finance and Entrepreneurship.
Previously, Jennifer was a Vice President at Park Lane Ventures, a healthcare-focused venture capital fund spun out of Essex Woodlands. Jennifer began her career as a consultant at Bain & Company in Chicago after graduating from Northwestern University.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.












