Since the first robot-assisted surgery was performed 35 years ago, there have been major advancements and refinements in robotic minimally invasive surgery. Today’s surgical robots are able to perform abdominal procedures with smaller incisions, reducing post-operative complications and improving patient outcomes.
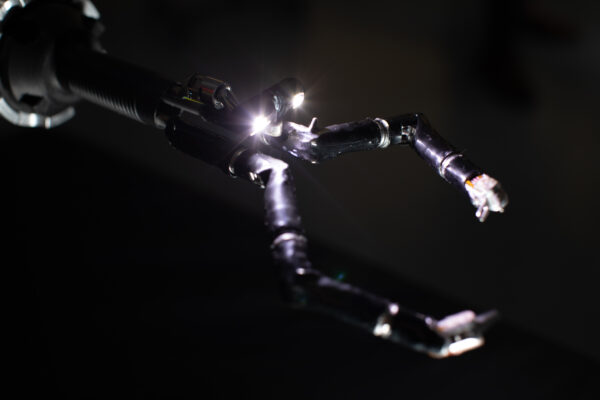
But just as important are the innovations around the collection of real-time data for interoperative feedback. Today’s surgical robots are equipped with dozens of miniature sensors which can measure force exerted, position and motion of the robot’s arms inside the patient. Imagine the benefits of a single incision robot that has full range of motion and mimics a surgeon’s hands, wrists, elbows and shoulders, facilitating unfettered access to critical anatomy. Additionally, this data will provide much needed insights and analysis into the true and accurate cost to treat the individual patient and population.

The Impact Brands: Empowering Wellness Through Natural and Holistic Solutions
In an era of escalating healthcare costs and a growing preference for natural, holistic approaches to health, The Impact Brands emerges as a collective of diverse brands dedicated to supporting overall wellness through natural means.
Robot-assisted surgery, and the data generated at scale from these miniaturized sensors, may be part of the solution to democratizing access to surgery and quality of care and enhancing knowledge sharing between surgeons of different experience levels.
Access to surgical care: a looming global crisis
The global gap between demand for surgical procedures and the available surgical workforce keeps widening. The AAMC projects that the world will face a shortage of surgeons across subspecialties (general surgery, obstetrics and gynecology, orthopedic surgery) of between 15,800 and 30,200 by 2034.
Simultaneously, the world population is aging – the proportion of people over the age of 65 will increase from 1 in 11 in 2019 to 1 in 6 in 2050. Demand for a range of surgical procedures, from hip replacement to cataract surgery to hernia repair, will soar.

When Investment Rhymes with Canada
Canada has a proud history of achievement in the areas of science and technology, and the field of biomanufacturing and life sciences is no exception.
There are two massive implications to this projected supply-demand challenge in surgery. First, unless something can be done to expand the surgical workforce, wait times for elective procedures could lengthen and patient outcomes could worsen. A 2016 Commonwealth Fund International Health Policy survey of 17 countries found that for elective surgeries, the wait times were about 140 days for a knee replacement and 110 days for a hip replacement. People waiting for a new hip or knee often have lower quality of life, sometimes needing to manage their pain with prescription medications or physical therapy. Imagine the health outcome consequences if these wait times increased.
The second implication is an unequal distribution of experienced surgeons in different regions or communities. Many young, talented surgeons are attracted to working at the big university hospitals, concentrated in urban areas, lured by the thrill and excitement of working in cutting-edge clinical and research settings. This leaves more rural areas underserved, with a reduced supply of surgical talent, further limiting access to quality care. Most acute is the shortage of general surgeons in rural areas, with some rural hospitals unable to meet patient needs for more complex surgeries.
With the need for knowledge-sharing so great, some surgeons are supplementing their training and prep by watching videos on YouTube demonstrating common procedures like a laparoscopic cholecystectomy. But the quality and professionalism of some of the videos are suspect.
How real-time data capture works
Let’s imagine a surgeon performing a robot-assisted ventral hernia repair on a patient. The surgeon, sitting at a surgeon console in the operating room, is able to view the data in real-time and understand how certain movements exerted by the robot’s arms cause an unacceptable amount of pressure and force on the surrounding tissue inside the abdominal cavity.
The surgeon can use that data to not only make better decisions for their patient in real-time, but also to make future robot-assisted procedures more accurate and reduce the chances of complications.
Imagine leveraging that data at scale. Applying artificial intelligence algorithms and data science, we can filter and process data to make the surgical community’s collective knowledge of minimally invasive ventral hernia repairs more robust. This would help inform better decision-making and improve accuracy in future surgeries. More pervasive use of surgical robotics and data collection could help to make access to quality surgical care more equal between wealthier and poorer communities. A surgeon based in a rural community hospital could benefit from data-driven best practices for a ventral hernia repair based on robotic-assisted surgeries performed hundreds or thousands of miles away. But this is only possible with the advanced sensing provided by today’s surgical robots.
Improving surgeon’s workloads
Democratization happens when we use technology to make something requiring expertise accessible to many more people. Democratization is happening in software with open source making it easier for many people to innovate together. It’s happening in manufacturing with 3D printing and in engineering with CAD. It can, and should, happen in surgery.
Surgical robots, and improvements to surgeries that come from data-driven knowledge sharing, can’t solve our looming surgeon shortage by themselves. We also need to expand the surgical workforce, while also making each surgeon’s workload more manageable.
Over time, surgical robots will help to automate more parts of surgical procedures – while improving patient experience and reducing complications – as we continue to leverage data from successful surgeries. More automation will free up surgeons from performing routine and rote tasks that make up a significant part of their workload, helping to reduce burnout and making a career in surgery even more desirable than it is today.
Our goal is not to enable a robot to perform complex surgeries without human involvement. But using surgical robotics to democratize access to quality care to underserved communities – using data-informed best practices – is an outcome that we can achieve and which the world needs.
Photo: Vicarious Surgical
Adam Sachs is CEO of Vicarious Surgical, a surgical robotics company he co-founded in 2014. Sachs leads the development and commercialization of the company’s surgical robots to increase the efficiency of procedures and improve patient outcomes. Prior to founding Vicarious Surgical, Sachs worked at Apple in manufacturing. He holds a Bachelor of Science in mechanical engineering from MIT and has worked for more than 11 years as a volunteer emergency medical technician for MIT EMS, an ambulance serving the MIT community.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.












